References:
[1] WHO. Trends
in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank
Group and the United Nations Population Division. Geneva: World Health Organization,
2019.
[2] Countdown
to 2015-decade report (2000–10): taking stock of maternal, newborn, and child survival.
Bhutta, Z. A., Chopra, M., Axelson, H., Berman, P., Boerma, T., Bryce, J, &
Wardlaw, T. 2015, The lancet, 375(9730), pp. 2032-2044.
[3] Global,
regional, and national levels of maternal mortality, 1990–2015: a systematic analysis
for the Global Burden of Disease Study 2015. Kassebaum, N. J., Barber, R. M., Bhutta,
Z. A., Dandona, L., Gething, P. W., Hay, S. I., & Ding, E. L. 2016, The Lancet,
388(10053)., pp. 1775-1812.
[4] The use
and perceived barriers of the partograph at public health institutions in East Gojjam
Zone, Northwest Ethiopia. Zelellw, D., Tegegne, T. 1, s.l.: Annals of global health,
2018, Vol. 84. 198.
[5] Global,
regional, and national levels and trends in maternal mortality between 1990 and
2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal
Mortality Estimation Inter-Agency Group. Alkema, L., Chou, D., Hogan, D., Zhang,
S., Moller, A. B., Gemmill, A., ... & Inter, U. N. M. M. E. 10017, s.l.: The
lancet, 2016, Vol. 387. 462-474.
[6] FMOH, EPHI.
National maternal death surveillance and response annual report 2008 EFY. s.l.:
Federal Democratic Republic of Ethiopia Ministry of Health (FMOH) EPHI, 2017.
[7] Indicators,
K. Mini Demographic and Health Survey. s.l.: EPHI and ICF, 2019.
[8] Level of
partograph utilization and its associated factors among obstetric caregivers at
public health facilities in East Gojam Zone, Northwest Ethiopia. Zelellw, D. A.,
& Tegegne, T. K. 2018, PloS one, 13(7).
[9] Magnitude
of partograph use and factors that affecting its utilization among obstetric caregivers
in public health institutions of West Showa Zone. Oromia Regional state, Ethiopia.
Willi, W. 2015.
[10] Effect of
partograph use on outcomes for women in spontaneous labour at term and their babies.
Lavender, T., Cuthbert, A., & Smyth, R. M. 2018, Cochrane Database of Systematic
Reviews, (8).
[11] Maternal
mortality from obstructed labor: a MANDATE analysis of the ability of technology
to save lives in sub-Saharan Africa. Harrison, M. S., Griffin, J. B., McClure, E.
M., Jones, B., Moran, K., & Goldenberg, R. L. 09, s.l.: American Journal
of Perinatology., 2016, Vol. 33. 873-881.
[12] The use
of the partograph in labor monitoring: a cross-sectional study among obstetric caregivers
in General Hospital, Calabar, Cross River State, Nigeria. Asibong, U., Okokon, I.
B., Agan, T. U., Oku, A., Opiah, M., Essien, E. J., & Monjok, E. s.l.: International
Journal of Women’s Health, 2014, Vol. 6. 873.
[13] Partograph
utilization as a decision-making tool and associated factors among obstetric care
providers in Ethiopia: a systematic review and meta-analysis. Ayenew, A. A., &
Zewdu, B. F. 1, s.l.: Systematic Reviews., 2020, Vol. 9. 251.
[14] Health professional’s
knowledge and use of the partograph in public health institutions in eastern Ethiopia:
a cross-sectional study. Mezmur, H., Semahegn, A., Tegegne, B. S. 1, s.l.: BMC
Pregnancy and Childbirth., 2017, Vol. 17. 1-7.
[15] A cross-sectional
study of partograph utilization as a decision-making tool for referral of abnormal
labour in primary health care facilities of Bangladesh. Khan, A. N. S., Billah,
S. M., Mannan, I., Mannan, I. I., Begum, T., Khan, M. A., & Graft-Johnson, J.
D. 2018, PloS one, 13(9).
[16] Knowledge
and utilization of the partograph: A cross-sectional survey among obstetric care
providers in urban referral public health institutions in northwe and southwest
Cameroon. Sama, C. B., Takah, N. F., Danwe, V. K., Melo, U. F., Dingana, T. N.,
& Angwafo III, F. F. 2017, PloS one 12(2).
[17] Knowledge
and utilization of the partograph among obstetric care givers in southwest Nigeria.
African journal of reproductive health. Fawole, A. O., Hunyinbo, K. I., & Adekanle,
D. A. 2008, African Journal of Reproductive Health, 12(1), pp. 22-29.
[18] Knowledge
and utilization of the partograph among midwives in the Niger Delta Region of Nigeria.
Opiah, M. M., Ofi, A. B., Essien, E. J., & Monjok, E. 2012, African Journal
of Reproductive Health, 16(1), pp. 125-132.
[19] Assessment
of knowledge and utilization of the partograph among health professionals in Amhara
region. Abebe, F., Birhanu, D., Awoke, W., Ejigu, T. 2, 2013, Ethiopia Science
Journal of Clinical Medicine, Vol. 2, pp. 26 - 42.
[20] Low utilization
of partograph and its associated factors among obstetric care providers in governmental
health facilities at West Shoa Zone, Central Ethiopia. Bedada, K. E., Huluka, T.
K., & Bulto, G. A. 2020, International Journal of Reproductive Medicine.
[21] Utilization
of the partograph and its associated factors among obstetric care providers in the
Eastern zone of Tigray, Northern Ethiopia. Gebreslassie, G. W., Weldegeorges, D.
A., Assefa, N. E., Gebrehiwot, B. G., Gebremeskel, S. G., Tafere, B. B., & Welesamuel,
T. G. 2019, The Pan African Medical Journal (34).
[22] Utilization
of Partograph and its associated factors among midwives working in public health
institutions, Addis Ababa City Administration, Ethiopia. Hagos, A. A., Teka, E.
C., & Degu, G. 2017, BMC Pregnancy and Childbirth, 20(1), pp. 1-9.
[23] Assessment
of partograph utilization and associated factors among obstetric care givers at
public health institutions in central zone, Tigray, Ethiopia. Hailu, T., Nigus,
K., Gidey, G., Hailu, B., & Moges, Y. 2018, BMC Research Notes, 11(1).,
pp. 1-6.
[24] Partograph
utilization and associated factors among obstetric care providers in North Shoa
Zone, Central Ethiopia: a cross sectional study. Wakgari, N., Amano, A., Berta,
M., & Tessema, G. A. 2015, African Health Sciences, 15(2), pp. 552-559.
[25] Partograph
Utilization and Associated Factors among Obstetric Care Providers Working in Public
Health Facilities of Wolaita Zone. Markos, M., Arba, A., & Paulos, K. 2020,
Journal of Pregnancy.
[26] Partograph
utilization and associated factors among obstetric care providers at public health
facilities in Hadiya Zone, Southern Ethiopia. Haile, Y., Tafese, F., Weldemarium,
T. D., & Rad, M. H. 2020, Journal of Pregnancy 2020.
[27] Knowledge
and utilization of partograph among health care professionals in public health institutions
of Bale zone, Southeast Ethiopia. Markos, D., & Bogale, D. 2016, Public health
(137), pp. 162-168.
[28] Knowledge
and utilization of partograph among obstetric care givers in public health institutions
of Addis Ababa, Ethiopia. Yisma, E., Dessalegn, B., Astatkie, A., & Fesseha,
N. 2013, BMC Pregnancy and Childbirth, 13(1), pp. 1-9.
[29] Partograph
utilization as a decision-making tool and associated factors among obstetric care
providers in Ethiopia: a systematic review and meta-analysis. Ayenew, A. A., &
Zewdu, B. F. 2020, Systematic Reviews, 9(1), pp. 1-11.
[30] Magnitude
of partograph use and associated factors among obstetric care givers in public health
institution in Sidama Zone, Southern Ethiopia. Eshetu, K., Hussen, E., & Dulla,
D. 6, s.l.: Diversity and Equality in Health and Care., 2017, Vol. 14.
[31] Effect of
partogram use on outcomes for women in spontaneous labour at term. Lavender, T.,
Hart, A., Smyth, R.M. s.l.: Cochrane Database Syst Rev., 2013, Vol. 7.
[32] Effect of
Partogram Use on Outcomes for Women in Spontaneous Labour at Term: RHL Commentary.
Soni, B. L. Geneva: World Health Organization, 2009, The WHO Reproductive Health
Library.
[33] Partograph
revisited. N., Magon. 1, 2011, Int J Clin Cases Investig, Vol. 3.
[34] Partograph
Utilization and Factors Associated with Poor Perinatal Outcomes in Wolaita Sodo
University Referral Hospital, Southern Ethiopia. Chemeda, G., Teklewold, B., &
Daka, K. s.l.: Journal of Health, Medicine, and Nursing., 2019, Vol. 63.
[35] Partograph
in management of labour. World Health Organization maternal health and safe motherhood
programme. WHO. s.l.: Lancet, 1994, Vol. 343. 1399-1404.
[36] Obstetric
care in low-resource settings: what, who, and how to overcome challenges to scale
up? Hofmeyr, G. J., Haws, R. A., Bergström, S., Lee, A. C., Okong, P., Darmstadt,
G. L., & Lawn, J. E. 2009, International Journal of Gynecology & Obstetric
(107)., pp. 21-45.
[37] Contemporary
patterns of spontaneous labor with normal neonatal outcomes. Zhang, J., Landy, H.
J., Branch, D. W., Burkman, R., Haberman, S., Gregory, K. D., ... & Reddy, U.
M. 2010, Obstetrics, and gynecology,116(6)., p. 1281.
[38] Labour,
W. P. P. (1994). A Practical Guide: The Partograph Part I, Principles and Strategy
WHO. World Health Organisation. Division of Family Health. Maternal Health and Safe
Motherhood Programme. Safe Motherhood Practical Guide: WHO/FHE/MSM/93.8. Labour,
W. P. P. s.l.: A Practical Guide: The Partograph Part I, Principles and Strategy
WHO. World Health Organisation. Division of Family Health. Maternal Health and Safe
Motherhood Programme. Safe Motherhood Practical Guide: WHO/FHE/MSM/93.8., 1994,
Safe Motherhood Practical Guide: WHO/FHE/MSM/93.8.
[39] Incidence
causes and outcome of obstructed labor in jimma university specialized hospital.
Fantu, S., Segni, H., & Alemseged, F. 2010, Ethiopian Journal of Health
Sciences, 20(3).
[40] The partograph
for the prevention of obstructed labor. Clinical obstetrics and gynecology, 52(2),
256-269. Mathai, M. 2009, Clinical obstetrics, and gynecology, 52(2)., pp. 256-269.
[41] Assessment
of knowledge and utilization of the partograph among health professionals in Amhara
region. Abebe, F., Birhanu, D., Awoke, W., Ejigu, T. 2, 2013, Ethiopia Science
Journal of Clinical Medicine, Vol. 2, pp. 26 - 42.
[42] Partograph
utilization and associated factors among obstetric care providers in North Shoa
Zone, Central Ethiopia: a cross sectional study. Wakgari, N., Amano, A., Berta,
M., & Tessema, G. A. 2, s.l.: African Health Sciences, 2015, Vol. 15.
552-559.
[43] Looking
into the performance-based financing black box: evidence from an impact evaluation
in the health sector in Cameroon. de Walque, Damien, et al. 6, 2021, Health Policy
and Planning, Vol. 36.
[44] Communities
of practice: the missing link for knowledge management on implementation issues
in low-income countries? Meessen, Bruno, et al. 8, 2011, Vol. 16.
[45] Performance-based
financing: the same is different. Meessen, Bruno, et al. 2017, Health Policy and
Planning.
[46] Output-based
payment to boost staff productivity in public health centres: contracting in Kabutare
District, Rwanda. Meessen, Bruno, Kashala, Jean-Pierre I and Musango, Laurent. 2007,
Bulletin of the World Health Organization, pp. 108-115.
[47] Effects
of pay for performance in health care: A systematic review of systematic reviews.
Eijkenaar, Frank, et al. 2-3, 2013, Health Policy, Vol. 110.
[48] Effect on
maternal and child health services in Rwanda of payment to primary health-care providers
for performance: an impact evaluation. Basinga, P., et al. 2011, The Lancet, pp.
1421-1428.
[49] Paying for
performance’ in Rwanda: Does it pay off? Kalk, A., Paul, F. A. and Grabosch, E.
2010, Tropical Medicine & International Health, pp. 182-190.
[50] Performance-based
financing for better quality of services in Rwandan health centres: 3-year experience.
Rusa, Louis, et al. 7, 2009, Tropical Medicine & International Health,
Vol. 14.
[51] A Conditional
Cash Transfer Program in the Philippines Reduces Severe Stunting. Kandpal, Eeshani,
et al. 9, 2016, The Journal of Nutrition, Vol. 146.
[52] Can performance-based
financing be used to reform health systems in developing countries? Ireland, Megan,
Paul, Elisabeth and Dujardin, Bruno. 9, 2011, Bulletin of the World Health Organization,
Vol. 89.
[53] Taking Results-Based
Financing from Scheme to System. Shroff, Zubin Cyrus, et al. 2, 2017, Health Systems
& Reform, Vol. 3.
[54] Why there
is so much enthusiasm for performance-based financing, particularly in developing
countries. Soeters, Robert and Vroeg, Piet. 9, 2011, Bulletin of the World Health
Organization, Vol. 89.
[55] The national
free delivery policy in Nepal: early evidence of its effects on health facilities.
Witter, S., et al. 2, 2011, Health Policy and Planning, Vol. 26.
[56] Studying
the link between institutions and health system performance: a framework and an
illustration with the analysis of two performance-based financing schemes in Burundi.
Bertone, M. P. and Meessen, B. 8, 2013, Health Policy and Planning, Vol. 28.
[57] Does training
on performance-based financing make a difference in performance and quality of health
care delivery? Health care provider’s perspective in Rungwe Tanzania. Manongi, Rachel,
et al. 1, 2014, BMC Health Services Research, Vol. 14.
[58] Performance-based
financing with GAVI health system strengthening funding in rural Cambodia: a brief
assessment of the impact. Matsuoka, S., et al. 4, 2014, Vol. 29.
[59] A realist
review to assess for whom, under what conditions and how pay for performance programmes
work in low- and middle-income countries. Singh, Neha S., et al. 2021, Social Science
& Medicine, Vol. 270.
[60] Didq: A
Command for Treatment-effect Estimation under Alternative Assumptions. Mora, Ricardo
and Reggio, Iliana. 3, 2015, The Stata Journal: Promoting Communications on Statistics
and Stata, Vol. 15.
[61] Use of the
partogram by doctors and midwives at Odi District Hospital, Gauteng, South Africa.
Maphashaa, O. M., Govender, I., Motloba, D. P., & Barua, C. 2017, South African
Family Practice, 59(2)., pp. 82-86.
[62] Use and
completion of partograph during labour is associated with a reduced incidence of
birth asphyxia: a retrospective study at a peri-urban setting in Ghana. Anokye,
R., Acheampong, E., Anokye, J., Budu-Ainooson, A., Amekudzie, E., Owusu, I., &
Mprah, W. K. 2019, Journal of Health, Population and Nutrition, 38(1)., pp. 1-8.
[63] Partograph
use among Midwives in the Gambia. Badjie, B., Kao, C. H., Gua, M. L., & Lin,
K. C. 2013, African Journal of Midwifery and Women’s Health, 7(2), pp. 65-69.
[64] Assessment
of partogram use during labour in rujumbura health Sub district, Rukungiri district,
Uganda. Ogwang, S., Karyabakabo, Z., & Rutebemberwa, E. 2009, African Health
Sciences, 9(2).
[65] Use of the
partogram by doctors and midwives at Odi District Hospital, Gauteng, South Africa.
Maphashaa, O. M., Govender, I., Motloba, D. P., & Barua, C. 2017, South African
Family Practice, 59(2), pp. 82-86.
[66] Helping
midwives in Ghana to reduce maternal mortality. Floyd, L. 2013, African Journal
of Midwifery and Women’s Health, 7(1), pp. 34-38.
[67] Care/Engender
Health, Fistula. Improving partograph use in Uganda through coaching and mentoring.
New York: Fistula Care., 2013.
[68] An exploration
of the unintended consequences of performance-based financing in 6 primary healthcare
facilities in Burkina Faso. Turcotte-Tremblay, A.M., Gali Gali, I.A., Ridde, V.
2, 2022, International Journal Health Policy Management., Vol. 11. 145–159.
[69] Partograph
utilization as a decision-making tool and associated factors among obstetric care
providers in Ethiopia: a systematic review and meta-analysis. Ayenew, A. A., &
Zewdu, B. F. 2020, Systematic reviews, 9(1)., p. 251.
[70] Partograph
utilization and associated factors among graduating health professional students
in Asella Referal and Teaching Hospital, Ethiopia, 2016. Bekele, D., Beyene, K.,
Hinkosa, L., & Shemsu, M. N. 2, s.l.: STM Journal., 2016, Vol. 6.
[71] Partograph
utilization and associated factors among obstetric care givers in governmental health
institutions of Jigjiga and Degehabur towns, Somali region, Ethiopia: A cross-sectional
study. Ayehubizu, L.M., Tibebeu, A.T., Fetene, M.T., Yohannes, S.H., Yadita, Z.S.
3, s.l.: PLoS ONE, 2022, Vol. 17.
[72] An evaluation
of the knowledge and utilization of the partogragh in primary, secondary, and tertiary
care settings in Calabar, South-South Nigeria. Okokon, I. B., Oku, A. O., Agan,
T. U., Asibong, U. E., Essien, E. J., & Monjok, E. 2014, International Journal
of Family Medicine 2014.
[73] De Walque,
D., Robyn, P. J., Saidou, H., Sorgho, G., Steenland, M. “de Walque, Damien; Robyn,
Paul Jacob; Saidou, Looking into the Performance-Based Financing Black Box: Evidence
from an Impact Evaluation in the Health Sector in Cameroon. Policy Research Working
Paper; No.8162. Washington D.C: World Bank, 2017.
[74] Local stakeholders’
perceptions about the introduction of performance-based financing in Benin: a case
study in two health districts. Paul, Elisabeth, Sossouhounto, Nadine and Eclou,
Dieudonné Sèdjro. 4, 2014, International Journal of Health Policy and Management,
Vol. 3.
[75] The effects
of performance-based financing on neonatal health outcomes in Burundi, Lesotho,
Senegal, Zambia, and Zimbabwe. Gage, Anna and Bauhoff, Sebastian. 3, 2021, Health
Policy and Planning, Vol. 36.
 Assessment of the Capacity of Patent and Proprietary Medicine Vendors to Provide Contraceptive Services to Adolescents in Kaduna State, NigeriaAuthor: Muhamma Murtala IbrahimDOI: 10.21522/TIJAR.2014.09.03.Art001
Assessment of the Capacity of Patent and Proprietary Medicine Vendors to Provide Contraceptive Services to Adolescents in Kaduna State, NigeriaAuthor: Muhamma Murtala IbrahimDOI: 10.21522/TIJAR.2014.09.03.Art001 Impact of Environmental Taxation on Environmental Sustainability in NigeriaAuthor: Joseph BrownDOI: 10.21522/TIJAR.2014.09.03.Art002
Impact of Environmental Taxation on Environmental Sustainability in NigeriaAuthor: Joseph BrownDOI: 10.21522/TIJAR.2014.09.03.Art002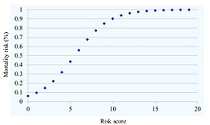 Predicting the Risk of in-Hospital Mortality in Patients with HIV-Associated Talaromyces Marneffei InfectionAuthor: Thanh Nguyen TatDOI: 10.21522/TIJAR.2014.09.03.Art003
Predicting the Risk of in-Hospital Mortality in Patients with HIV-Associated Talaromyces Marneffei InfectionAuthor: Thanh Nguyen TatDOI: 10.21522/TIJAR.2014.09.03.Art003 Assessing Teachers’ Knowledge in Analysing Errors in Mathematical Word Problems of Ghanaian Primary School PupilsAuthor: Stella Sitsofe Yawa AsaseDOI: 10.21522/TIJAR.2014.09.03.Art004
Assessing Teachers’ Knowledge in Analysing Errors in Mathematical Word Problems of Ghanaian Primary School PupilsAuthor: Stella Sitsofe Yawa AsaseDOI: 10.21522/TIJAR.2014.09.03.Art004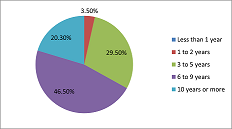 The Influence of Media on Voting Behavior in Ghana: The Case in Western North RegionAuthor: Isaac DampteyDOI: 10.21522/TIJAR.2014.09.03.Art005
The Influence of Media on Voting Behavior in Ghana: The Case in Western North RegionAuthor: Isaac DampteyDOI: 10.21522/TIJAR.2014.09.03.Art005 An Assessment of Healthcare Relationship Trust between Patent Medicine Vendors and Residents of Hard-to-Reach Settlements in Northern NigeriaAuthor: Oluwasegun John IbitoyeDOI: 10.21522/TIJAR.2014.09.03.Art006
An Assessment of Healthcare Relationship Trust between Patent Medicine Vendors and Residents of Hard-to-Reach Settlements in Northern NigeriaAuthor: Oluwasegun John IbitoyeDOI: 10.21522/TIJAR.2014.09.03.Art006 Utilization of Information Resources and Services among Undergraduate Students in Federal University Libraries in South-South, NigeriaAuthor: Ebaye A.SDOI: 10.21522/TIJAR.2014.09.03.Art007
Utilization of Information Resources and Services among Undergraduate Students in Federal University Libraries in South-South, NigeriaAuthor: Ebaye A.SDOI: 10.21522/TIJAR.2014.09.03.Art007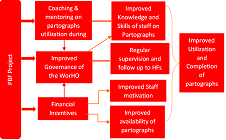 Impact of Performance-Based Financing (PBF) Program on Utilization and Completeness of Partographs in JimmaAuthor: Polite DubeDOI: 10.21522/TIJAR.2014.09.03.Art008
Impact of Performance-Based Financing (PBF) Program on Utilization and Completeness of Partographs in JimmaAuthor: Polite DubeDOI: 10.21522/TIJAR.2014.09.03.Art008 An Analysis of the Media in the Generation of Electoral Conflict Behaviours among Voters in the Western North Region, GhanaAuthor: Isaac DampteyDOI: 10.21522/TIJAR.2014.09.03.Art009
An Analysis of the Media in the Generation of Electoral Conflict Behaviours among Voters in the Western North Region, GhanaAuthor: Isaac DampteyDOI: 10.21522/TIJAR.2014.09.03.Art009 Exploring the Understanding of Technical University Lecturers on Continuous Professional Development in GhanaAuthor: William Owusu-BoatengDOI: 10.21522/TIJAR.2014.09.03.Art010
Exploring the Understanding of Technical University Lecturers on Continuous Professional Development in GhanaAuthor: William Owusu-BoatengDOI: 10.21522/TIJAR.2014.09.03.Art010 Supervisor-Supervisee Relations and Job Performance: Study of Healthcare Field Officers in Chongwe, ZambiaAuthor: Dalitso MasekoDOI: 10.21522/TIJAR.2014.09.03.Art011
Supervisor-Supervisee Relations and Job Performance: Study of Healthcare Field Officers in Chongwe, ZambiaAuthor: Dalitso MasekoDOI: 10.21522/TIJAR.2014.09.03.Art011 Collection Development Variables and Use of Library Materials in Academic Libraries in South-South Geo-political Zone of NigeriaAuthor: Ebaye A.SDOI: 10.21522/TIJAR.2014.09.03.Art012
Collection Development Variables and Use of Library Materials in Academic Libraries in South-South Geo-political Zone of NigeriaAuthor: Ebaye A.SDOI: 10.21522/TIJAR.2014.09.03.Art012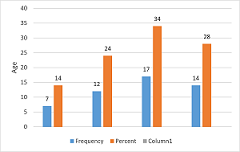 Cancer Screening Technology and Attitude of Women Towards Cervical CancerAuthor: Ayesha IramDOI: 10.21522/TIJAR.2014.09.03.Art013
Cancer Screening Technology and Attitude of Women Towards Cervical CancerAuthor: Ayesha IramDOI: 10.21522/TIJAR.2014.09.03.Art013 Evaluating the Implementation of Components of the Performance Management System in the Zambian Public Service: A Case Study of Development Bank of ZambiaAuthor: Charles Tennard BandaDOI: 10.21522/TIJAR.2014.09.03.Art014
Evaluating the Implementation of Components of the Performance Management System in the Zambian Public Service: A Case Study of Development Bank of ZambiaAuthor: Charles Tennard BandaDOI: 10.21522/TIJAR.2014.09.03.Art014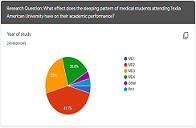 The Correlation between Sleeping Patterns and Academic Performance for TAU Medical StudentsAuthor: Tiffany ErebeDOI: 10.21522/TIJAR.2014.09.03.Art015
The Correlation between Sleeping Patterns and Academic Performance for TAU Medical StudentsAuthor: Tiffany ErebeDOI: 10.21522/TIJAR.2014.09.03.Art015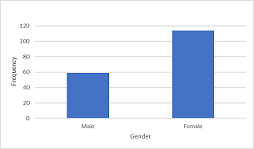 A Comparison of Students’ Attitude and Perception towards Morning or Afternoon Classes in Texila American University, 2021Author: Ramona AdamsDOI: 10.21522/TIJAR.2014.09.03.Art016
A Comparison of Students’ Attitude and Perception towards Morning or Afternoon Classes in Texila American University, 2021Author: Ramona AdamsDOI: 10.21522/TIJAR.2014.09.03.Art016 Angle of Humeral Torsion: Comparative Analysis with Length and Mid-Shaft CircumferenceAuthor: Subodh Kumar YadavDOI: 10.21522/TIJAR.2014.09.03.Art017
Angle of Humeral Torsion: Comparative Analysis with Length and Mid-Shaft CircumferenceAuthor: Subodh Kumar YadavDOI: 10.21522/TIJAR.2014.09.03.Art017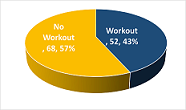 The Effect of a Systematic Workout Routine on Medical Students’ General Wellbeing and Academic Performance at the Texila American UniversityAuthor: Lianne RickfordDOI: 10.21522/TIJAR.2014.09.03.Art018
The Effect of a Systematic Workout Routine on Medical Students’ General Wellbeing and Academic Performance at the Texila American UniversityAuthor: Lianne RickfordDOI: 10.21522/TIJAR.2014.09.03.Art018 A Review of Cooking Oils (Coconut and Palm Oil) as Blood Plasma RegulatorAuthor: Aminuddin MohammadDOI: 10.21522/TIJAR.2014.09.03.Art019
A Review of Cooking Oils (Coconut and Palm Oil) as Blood Plasma RegulatorAuthor: Aminuddin MohammadDOI: 10.21522/TIJAR.2014.09.03.Art019
