References:
[1]
Müller, O., & Krawinkel,
M. (2005). Malnutrition and Health in Developing Countries. Canadian Medical
Association Journal, 279-286.
[2]
Semahegn, A., Tesfaye, G.,
& Bogale, A. (2014). Complementary feeding practice of mothers and associated
factors in Hiwot Fana Specialized Hospital, Eastern Ethiopia. Pan African Medical
Journal, 1-11.
[3]
Beyene, T. (2012). Predictors
of nutritional status of children visiting health facilities in Jimma zone, South
West Ethiopia. nt. J. Adv. Nurs. Sci. Pract., 1-13.
[4]
Rahim, F. (2014). Risk factors
of underweight in children aged 7-59 months. J. Public Health, 115-121.
[5]
Kassa, T., Meshesha, B., Haji,
Y., & Ebrahim, J. (2016). Appropriate complementary feeding practices and associated
factors among mothers of children age 6–23 months in Southern Ethiopia, 2015. BMC
Pediatrics.
[6]
Amsalu, S. &. Tigabu,
Z (2008). : Risk factors for severe acute malnutrition in children under the age
of five: A case-control study, Journal of Health Development, 1-96 Vol 22(1).
[7]
Daelmans, B., Ferguson, E., Lutter, C. K., Singh,
N., Pachón, H., Creed-kanashiro, H., & Briend, A. (2013). Designing appropriate
complementary feeding recommendations: Tools for programmatic action. Martenal
& Child Nutrition, 116-130.
[8]
Mesfin, A., Henry, C., Girma,
M., & Whiting, S. J. (2015). Use of pulse crops in complementary feeding of
6–23 months old infants and young children in Taba Kebele, Damot Gale District,
Southern Ethiopia. Southern Ethiopia. Journal of Public Health Africa, 1-6.
[9]
Khanal, V., Sauer, K., &
Zhao, Y. (2013). Determinants of complementary feeding practices among Nepalese
children aged 6–23 months: Findings from demographic and health survey 2011. BMC
Pediatrics, 1-13.
[10]
Shi, L., & Zhang, J. (2011). Recent evidence of the effectiveness of educational interventions
for improving complementary feeding practices in developing countries, Journal
of Tropical Pediatrics, 57, 91-98.
[11]
Das, N., Chattopadhyay, D.,
Chakraborty, S., & Dasgupta, A. (2013). Infant and Young Child Feeding Perceptions
and Practices among Mothers in a Rural Area of West Bengal, India. Annals of
medical and health sciences research., 370-375.
[12]WHO. (2003). : Global strategy for infant and young child feeding.
Geneva: World health Organization.
[13]
Hackett, K., Mukta, U., Jalal,
C., & Sellen, D. (2015). Knowledge, attitudes and perceptions on infant and
young child nutrition and feeding among adolescent girls and young mothers in rural
Bangladesh. Maternal & child nutrition, 173-189.
[14]
Sawaya, A. L. (2006). Malnutrition:
long term consequences and nutritional recovery effects. Estudos Avançados, 147-158.
[15]
Burns, C. E., Brady, M. A.,
& Dunn, A. M. (2000). Pediatric Primary Care, A Hand Book for Nurse Pediatricians
(2nd edition). New York: Elsevier.
[16]
Kliegman, R. B., Stanton,
Geme, J. S., Schor, N. F., & Behrman, R. E. (2011). NALSON text book of Pediatric.
Philadephia: Sounders.
[17]
UNICEF. (2010). Indicators
for assessing infant and young child feeding practices, New York: UNICEF.
[18]
WFP. (2009). Emergency Food
Security Assessment Handbook. Rome, World Food Programme.
[19]
WHO. (2014). Comprehensive
Implementation Plan on Maternal, Infant and Young Child Nutrition. Geneva: World
Health Organization.
[20]
WHO., & UNICEF. (2003).
Global strategy for infant and young child feeding. Geneva: WHO.
[21]
Saha, K. K., Frongillo, E.
A., Alam, D. S., Arifeen, S. E., Persson, L. Å., & Rasmussen, K. M. (2008).
Appropriate infant feeding practices result in better growth of infants and young
children in rural Bangladesh. American Journal of Clinical Nutrition, 1852-1859.
[22]
Turyashemererwa, F. (2009).
Prevalence of early childhood malnutrition and influencing factors in peri urban
areas of Kabarole district, Western Uganda. African Journal of Food Agriculture
Nutrition and Development, 975-989.
[23]
Azizi, M., Aghaee, N., Ebrahimi,
M., & Ranjbar, K. (2011). Nutrition knowledge, the attitude and practices of
college students. Facta Universitatis, 349-357.
[24]
Azizi, M., Aghaee, N., Ebrahimi,
M., & Ranjbar, K. (2011). Nutrition knowledge, the attitude and practices of
college students. Facta Universitatis, 349-357.
[25]
Mowe, M., Bosaeus, I., &
Højgaard, H. (2008). Insufficient nutritional knowledge among health care workers?
Insufficient nutritional knowledge among health care workers? Clinical Nutrition,
196-202.
[26]
Bukusuba, J., Kikafunda, J.
K., & Whitehead, R. G. (2010). Nutritional knowledge, attitudes, and practices
of women living with HIV in Eastern Uganda. Journal of Health, Population, and
Nutrition, 182-188.
[27]
Ray, S., Mishra, R., Biswa,
R., Kumar, R., Halden, A., & Chattrjee, T. (1999). Nutritional status of pavement
dweller children of Calcutta city. Indian J Public Health, 49-54. 29.
[28]
Caulfield, L., Huffman, S.,
& Piwoz, E. (1999). Interventions to improve intake of complementary foods by
infants 6 to 12 months of age in developing countries: impact on growth and on trie
prevalence of malnutrition and potential contribution to child survival. Food Nutr
Bull, 183-200.
[29]
Abiyu, C., & Belachew,
T. (2020). Level and Predictors of Mothers’ Knowledge and Attitude on Optimal Complementary
Feeding in West Gojjam Zone, Northwest Ethiopia. Nutrition and Dietary Supplements,
113-121.
[30]
WHO, USAID, AED, UCDAVIS,
& IFPRI:. (2010). Indicators for assessing infant and young child feeding practices.
Geneva: WHO.
[31]
WHO. (2014). WHO recommendations
on postnatal care of the mother and new-born. Geneva: World Health Organization.
[32]
Donna, M. (2012). The first
month: Feeding and Nutrition. American Academy of Pediatrics.
[33]
De Carvalho, M., Robertson,
S., Friedman, A., & Klaus, M. (1983). Effect of frequent breastfeeding on early
milk production and infant weight gain. Pediatrics, 72(3):307-11.
[34]
Anderson, G., Moore, E., Hepworth,
J., & Bergman, N. ( 2003.). Early skin-to-skin contact for mothers and their
healthy new-born infants (Cochrane Review). In: The Cochrane Library, Issue
2 2003. Oxford: Update Software.
[35]
Kostandy, R., Anderson, G.,
& Good, M. (2013). Skin-to-skin contact diminishes pain from hepatitis B vaccine
injection in healthy full-term neonates. Neonatal Network, 32(4):274-80.
[36]
36. Beijers, R., Cillessen,
L., & Zijlmans, M. ( 2016 ). 2016. opens in a new window. An experimental study
on mother-infant skin-to-skin contact in full-terms. Infant Behav Dev., 43:58-65.
[37]
Dewar, G. (2019). Breastfeeding
on demand: Benefits, questions, and evidence-based tips. Parenting Science.
[38]
Iacovou, M., & Sevilla,
A. ( 2013. ). Infant feeding: the effects of scheduled vs on-demand feeding on mothers’
wellbeing and children’s cognitive development. Eur J Public Health., 23(1):13-9.
[39]WHO/UNICEF. (2009). Baby-Friendly Hospital Initiative: Revised,
updated, and expanded for integrated care. Geneva, Switzerland: World Health
Organization.
[40]Buckley, S. J. (2014 ). The hormonal physiology of childbearing.
New York, NY: Childbirth Connection.
[41]Moore, E., Anderson, G., Bergman, N., & Dowswell, T. (2012).
Early skin-to-skin contact for mothers and their healthy new-born infants. Cochrane
Database Syst Rev.
[42]
Widström, A., Lilja, G., Aaltomaa-Michalias,
P., Dahllöf, A., Lintula, M., & Nissen, E. (2011 ). New-born behaviour to locate
the breast when skin-to-skin: a possible method for enabling early self-regulation.
Acta Paediatr. , 100(1):79-85.
[43]
National Demographic Health
Survey, Nigeria Bureau of Statistics (2018).
[44]
Takahashi, K., Ganchimeg,
T., Ota, E., Vogel, J., Souza, J., & Laopaiboon, M. (2017). Prevalence of early
initiation of breastfeeding and determinants of delayed initiation of breastfeeding:
secondary analysis of the WHO Global Survey. Sci Rep.
[45]
Edmond, K., Zandoh, C., Quigley,
M., Amenga-Etego, S., Owusu-Agyei, S., & Kirkwood, B. (2006). Delayed breastfeeding
initiation increases the risk of neonatal mortality. Pediatrics., e360-e6.
[46]
Multiple Indicator Cluster
Survey, Nigeria Bureau of Statistics (2016-2017).
[47]
Group, N. (2016). Timing of
initiation, patterns of breastfeeding, and infant survival: prospective analysis
of pooled data from three randomised trials. Lancet Glob Health, 4(4):e266–75.
[48]
M'Rabet, L., Vos, A., Boehm,
G., & Garssen, J. (2008). Breast-feeding and its role in the early development
of the immune system in infants: consequences for health later in life. J Nutr,
138(9):1782S–90S.
[49]
Patil, C., Turab, A., Ambikapathi,
R., Nesamvuni, C., Chandyo, R., & Bose, A. (2015). Early interruption of exclusive
breastfeeding: results from the eight-country MAL-ED study. J Health Popul Nutr,
34:10. 50.
[50]
Ballard, O., & Morrow,
A. (2013). Human milk composition: nutrients and bioactive factors. Pediatr Clin
North Am, 60(1):49–74.
[51]
Toscano, M., De Grandi, R.,
Grossi, E., & Drago, L. (2017). Role of the Human Breast Milk-Associated Microbiota
on the New-borns’ Immune System: A Mini-Review. Front Microbiol., 8:2100.
[52]
Hassiotou, F., Hepworth, A.,
Metzger, P., Lai, C., Trengove, N., Hartmann, P., & Filgueira, L. (2013). Maternal
and infant infections stimulate a rapid leukocyte response in breastmilk. Clin
Transl Immunology, 2(4):e3.
[53]
Pribylova, J., Krausova, K.,
Kocourkova, I., Rossmann, P., Klimesova, K., Kverka, M., & Tlaskalova-Hogenova,
H. (2012). Colostrum of healthy mothers contains broad spectrum of secretory IgA
autoantibodies. J Clin Immunol, 32(6):1372-1380.
[54]
Bode, L. (2012). Human milk
oligosaccharides: every baby needs a sugar mama. Glycobiology.
[55]
Williamson, N. (1990). Breastfeeding
trends and the breastfeeding promotion programme in the Philippines. Asia-Pac
Pop Journal, 5: 113-124.
[56]
Hanks, J. (1963). Maternity
and its rituals in Bang Chan. Southeast Asia Program, Department of Asian Studies.
Ithaca: Cornell University., Data Paper No. 51.
[57]
Bhale, P., & Jain, S.
(1999). Is colostrum really discarded by Indian mothers? Indian Pediatr,
36: 1069-1070.
[58]
Goyale, A., Jain, P., Vyas,
S., Saraf, H., & Shekhawat, N. (2004). Colostrum and Prelacteat Feeding Practices
Followed by Families of Pavement and Roadside Squatter Settlements. Indian J
Prev Soc Med., 35 (1&2): 58-62.
[59]
Morse, J., Jehle, C., &
Gamble, D. (1990). Initiating breast-feeding: a world survey of the timing of postpartum
breastfeeding. Int J Nurs Stud., 27: 303-313.
[60]
Duong, D., Binns, C., &
Lee, A. (2004). Breastfeeding initiation and exclusive breastfeeding in rural Vietnam.
Public Health Nutr., 7: 795-799.
[61]
Omotola, B., & Akinyele,
I. (1985). Infant feeding practices of urban low-income group in Ibadan. Nutr
Rep Int, 31:837-848.
[62]
Osrin, D., Tumbahangphe, K.,
Shrestha, D., Mesko, N., Shrestha, B., Manandhar, M., Costello, A. (2002). Cross-sectional,
community-based study of care of new-born infants in Nepal. BMJ, 325(7372):1063.
[63]
Fikree, F., Ali, T., Durocher,
J., & Rahbar, M. (2005). New-born care practices in low socio-economic settlements
of Karachi, Pakistan. Soc Sci Med., 60(5): 911-921.
[64]
Jethi, S., & Shriwastava,
D. (1987). Knowledge, attitudes and practices regarding infant feeding among mothers.
Indian Pediatr, 24: 921-924.
[65]
Agrawal, D., Agrawal, K.,
& Khare, B. (1985). Study on Current Status of infant and childhood feeding
practices. Indian Pediatr , 22: 716.
[66]
Weldesamuel, G., Atalay, H.,
Zemichael, T., Gebre, H., Abraha, D., & Amare, A. (2018). Colostrum avoidance
and associated factors among mothers having children less than 2 years of age in
Aksum town Tigray, Ethiopia: a cross-sectional study. BMC research notes,
11(1):601.
[67]
Shewasinad, S., Manjura, M.,
Bolesh, A., Sisay, D., & Negash, S. (2017). Assessment of knowledge, attitude
and practice towards colostrum feeding among antenatal care attendant pregnant mothers
in Mizan Tepi University Teaching Hospital, Bench Maji Zone, SNNPR, South West Ethiopia.
J Preg Child Health., 4:348.
[68]
Legesse, M., Demena, M., Mesfin,
F., & Haile, D. (2015). Factors associated with colostrum avoidance among mothers
of children aged less than 24 months in Raya Kobo district, North-eastern Ethiopia:
community-based cross-sectional study. Journal of tropical pediatrics, 61(5):357–63.
[69]
Ayalew, T. (2020). Exclusive
breastfeeding practice and associated factors among first-time mothers in Bahir
Dar city, north West Ethiopia, removed: a community-based cross-sectional study.
Heliyon, 6:9.
[70]
Ozelci, P., Elmaci, N., &
Ertem, M. S. (2006). Breastfeeding beliefs and practices among migrant mothers in
slums of Diyarbakir, Turkey, 2001. European Journal of Public Health, 16(2):
143-148.
[71]Petit, A. (2008). Perception and Knowledge on Exclusive
Breastfeeding among Women Attending Antenatal and Postnatal Clinics A Study
from Mbarara Hospital – Uganda. Tanzania: Tanzania Medical Students’ Association.
[72]
Ojong, n., &
Chukwudozie, C. (2019). Exclusive Breastfeeding Perception and Practice among
Nursing Mothers Attending Infant Welfare Clinic in a Secondary Health Facility
in Southern Nigeria. African Journal of Health, Nursing and Midwifery,
2(1): 22-34.
[73]
WHO. (1991). Indicators for
assessing infant and young child feeding practices. Washington D.C: World Health
Organization.
[74]
Ogbo, F., Page, A., Idoko,
J., Claudio, F., & Agho, K. (2016). Diarrhoea and suboptimal feeding practices
in Nigeria: evidence from the national household surveys. Paediatr Perinat Epidemiol,
30:346–55.
[75]
Ogbo, F., Agho, K., Ogeleka,
P., Woolfenden, S., Page, A., & Eastwood, J. (2017). Infant feeding practices
and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PLoS
One., 12(2):e017179276.
[76]
WHO. (2008). Training course
on child growth assessment. Geneva: WHO.
[77]
WHO. (1991). Indicators for
accessing breastfeeding practices. Geneva: World Health Organization. 7.
[78]
Pahhani, Z., Salem, R., Lassi,
Z., Siddiqui, F., Keats, E., Das, J., Bhutta, Z. (2021). Optimal Timing of Introduction
of Complementary feeding: Protocol for a systematic review and meta-analysis. Research
Square, 1-14.
[79]
Chiang, K., Hamner, H., Li,
R., & Perrine, C. (2020). Timing of Introduction of Complementary Foods - United
States, 2016-2018. Washington: US Department of Health and Human Services/Centers
for Disease Control and Prevention.
[80]
Inoue, M., & Binns, C.
(2014). Introducing solid foods to infants in the Asia Pacific region. Nutrients.,
6(1):276-88.
[81]
Dhami, M., Ogbo, F., Osuagwu,
U., & Agho, K. (2019). Prevalence and factors associated with complementary
feeding practices among children aged 6–23 months in India: a regional analysis.
BMC public health, 19(1):1034.
[82]
Saaka, M., Larbi, A., Mutaru,
S., & Hoeschle-Zeledon, I. (2016). Magnitude and factors associated with appropriate
complementary feeding among children 6–23 months in northern Ghana. BMC Nutrition.,
2(1):2.
[83]
Sisay, W., Edris, M., &
Tariku, A. (2016). Determinants of timely initiation of complementary feeding among
mothers with children aged 6–23 months in Lalibela District, Northeast Ethiopia.
BMC public health., 16(1):884.
[84]
English, L., Obbagy, J., Wong,
Y., Butte, N., Dewey, K., & Fox, M. (2019). Types and amounts of
complementary foods and beverages consumed and growth, size, and body composition:
a systematic review. The American journal of clinical nutrition., 109(Supplement_1):956S-77S.
.jpg)
 Making FIFA World Cup Qatar 2022 Truly Healthy and Safe: Strategies and Legacy for Present and Future Sporting EventsAuthor: Abiodun Bamidele AdelowoDOI: 10.21522/TIJAR.2014.SE.22.02.Art001
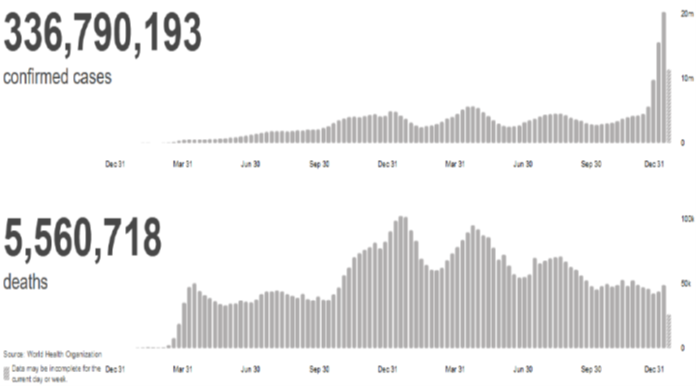
Making FIFA World Cup Qatar 2022 Truly Healthy and Safe: Strategies and Legacy for Present and Future Sporting EventsAuthor: Abiodun Bamidele AdelowoDOI: 10.21522/TIJAR.2014.SE.22.02.Art001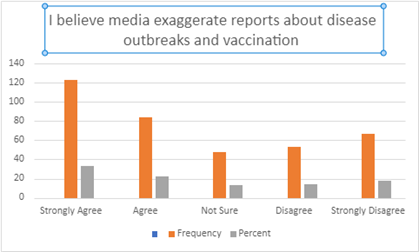 Epidemics and Vaccination Dilemma in Complex Networks: A Case Study of Kosefe and Shomolu Local Government Area Lagos NigeriaAuthor: Odis Adaora IsabellaDOI: 10.21522/TIJAR.2014.SE.22.02.Art002
Epidemics and Vaccination Dilemma in Complex Networks: A Case Study of Kosefe and Shomolu Local Government Area Lagos NigeriaAuthor: Odis Adaora IsabellaDOI: 10.21522/TIJAR.2014.SE.22.02.Art002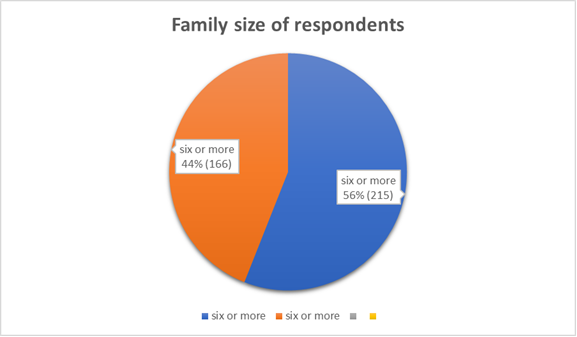 Predictors of Family Size Among Men in Urban Slums of Enugu, Southeast Nigeria: A Cross Sectional StudyAuthor: Enebe NODOI: 10.21522/TIJAR.2014.SE.22.02.Art003
Predictors of Family Size Among Men in Urban Slums of Enugu, Southeast Nigeria: A Cross Sectional StudyAuthor: Enebe NODOI: 10.21522/TIJAR.2014.SE.22.02.Art003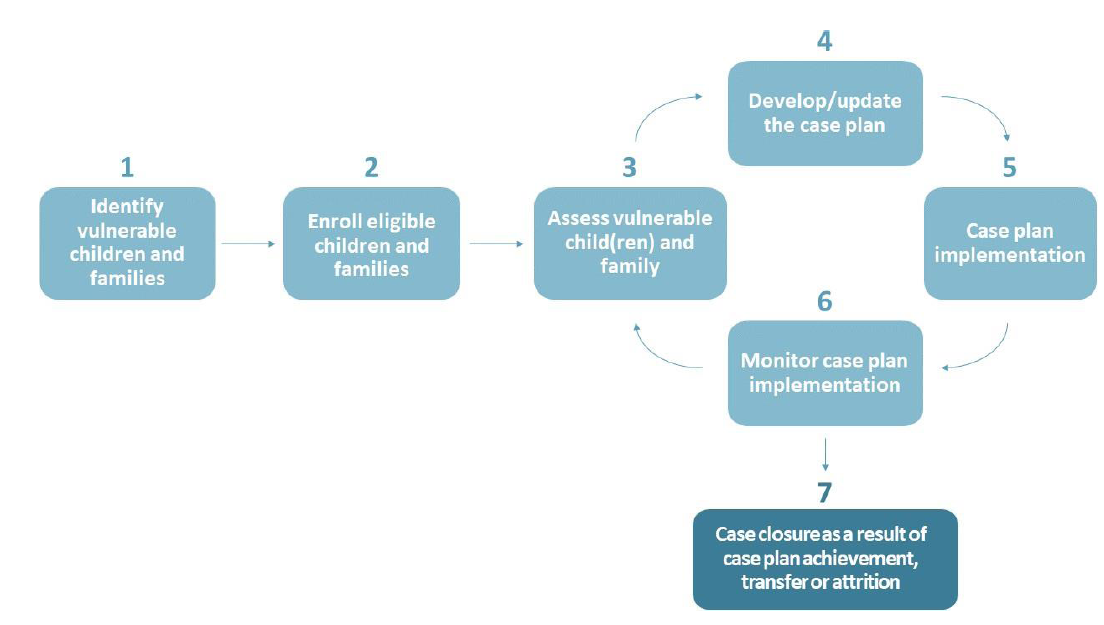 Investigating the Effectiveness of Case Management among Orphans and Vulnerable Children at Household Level in Enugu State, NigeriaAuthor: Prince O. EzekielDOI: 10.21522/TIJAR.2014.SE.22.02.Art005
Investigating the Effectiveness of Case Management among Orphans and Vulnerable Children at Household Level in Enugu State, NigeriaAuthor: Prince O. EzekielDOI: 10.21522/TIJAR.2014.SE.22.02.Art005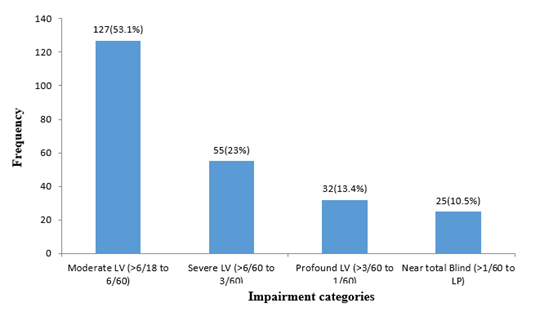 Characteristics of the Low Vision Population in South-East NigeriaAuthor: Precious Chidozie AzubuikeDOI: 10.21522/TIJAR.2014.SE.22.02.Art008
Characteristics of the Low Vision Population in South-East NigeriaAuthor: Precious Chidozie AzubuikeDOI: 10.21522/TIJAR.2014.SE.22.02.Art008 Outcome of Community-Initiated Treatment of Drug-Resistant Tuberculosis Patients in Akwa Ibom State, NigeriaAuthor: Asuquo, E. A.DOI: 10.21522/TIJAR.2014.SE.22.02.Art011
Outcome of Community-Initiated Treatment of Drug-Resistant Tuberculosis Patients in Akwa Ibom State, NigeriaAuthor: Asuquo, E. A.DOI: 10.21522/TIJAR.2014.SE.22.02.Art011 Protective Masks: A Semiotic Discourse in Times of PandemicAuthor: Kundlata MishraDOI: 10.21522/TIJAR.2014.SE.22.02.Art019
Protective Masks: A Semiotic Discourse in Times of PandemicAuthor: Kundlata MishraDOI: 10.21522/TIJAR.2014.SE.22.02.Art019 The Perceived Quality of Life amongst Diabetic Patients Attending the Outpatient Department at a District Hospital in South AfricaAuthor: Elizabeth RejiDOI: 10.21522/TIJAR.2014.SE.22.02.Art020
The Perceived Quality of Life amongst Diabetic Patients Attending the Outpatient Department at a District Hospital in South AfricaAuthor: Elizabeth RejiDOI: 10.21522/TIJAR.2014.SE.22.02.Art020 The Impact of Moderated WhatsApp Text Messaging for Improving Maternal and New-born Referral Outcomes among Health Facilities in Luapula Province, ZambiaAuthor: Lweendo MunzeleDOI: 10.21522/TIJAR.2014.SE.22.02.Art021
The Impact of Moderated WhatsApp Text Messaging for Improving Maternal and New-born Referral Outcomes among Health Facilities in Luapula Province, ZambiaAuthor: Lweendo MunzeleDOI: 10.21522/TIJAR.2014.SE.22.02.Art021 Knowledge, Attitudes and Perceptions of Women of Child-Bearing Age Group on Abortion Services, Case Study Location Clinic, Kasama District, Northern, ZambiaAuthor: Fredrick MwilaDOI: 10.21522/TIJAR.2014.SE.22.02.Art022
Knowledge, Attitudes and Perceptions of Women of Child-Bearing Age Group on Abortion Services, Case Study Location Clinic, Kasama District, Northern, ZambiaAuthor: Fredrick MwilaDOI: 10.21522/TIJAR.2014.SE.22.02.Art022 Impact of Covid-19 Pandemic on Clinical and Non-Clinical Staff Working in United Nations in BurundiAuthor: Jean Claude MusengimanaDOI: 10.21522/TIJAR.2014.SE.22.02.Art023
Impact of Covid-19 Pandemic on Clinical and Non-Clinical Staff Working in United Nations in BurundiAuthor: Jean Claude MusengimanaDOI: 10.21522/TIJAR.2014.SE.22.02.Art023
