Anticolitis Activity of Myrobalan Powder via Regulating Colonic Enterochromaffin Cells and Serotonin
Abstract:
Objective: To investigate whether Myrobalan powder
has an anti-inflammatory effect on colonic inflammation and to explore the mechanism
involved.
Materials and
Methods: Myrobalan
powder was orally administrated to trinitrobenzene sulfonic acid (TNBS)-induced
colitis mice at the dose of 3, 6, and 12 g/kg/d for 7 consecutive days. Body weight,
stool consistency, histopathological score, and myeloperoxidase (MPO) activity were
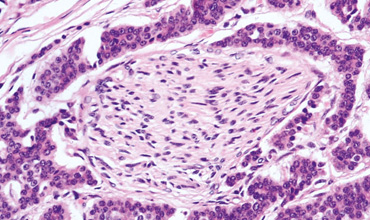
tested to evaluate the effect of Myrobalan powder on colonic inflammation while
colonic enterochromaffin (EC) cell density and serotonin 5-hydroxytryptamine (5-HT)
content were investigated to identify the effect of Myrobalan powder on colonic
5-HT availability.
Results: The results showed that the body weight
of colitis mice was markedly decreased by 10, 12, 14, and 17% at 1, 3, 5, and 7
days (P< 0.05), whereas stool
consistency score (3.6 vs. 0.4, P<
0.05), histopathological score (3.6 vs. 0.3, P< 0.05), and MPO activity (2.7 vs. 0.1,P< 0.05) in colitis mice were significantly
increased compared to that of the normal mice; Myrobalan powder treatment dose-dependently
increased the body weight (7–13% increase) and decreased the stool consistency score
(0.4–1.4 decrease), histopathological score (0.2–0.7 decrease), and MPO activity
(0.1–0.9 decrease) in colitis mice. Colonic EC cell density (70% increase) and 5-HT
content (40% increase) were markedly increased in colitis mice (P< 0.05), Myrobalan powder treatment
dose-dependently reduced EC cell density (20–50% decrease), and 5-HT content (5–27%
decrease) in colitis mice.
Conclusion: The findings demonstrate that the anti-inflammatory
effect of Myrobalan powder on TNBS - induced colitis may be mediated via reducing
EC cell hyperplasia and 5-HT content. The important role of Myrobalan powder in
regulating colonic EC cell number and 5-HT content may provide an alternative therapy
for colonic inflammation.
Keywords: Colonic inflammation, enterochromaffin
cell, serotonin, ulcerative colitis
References:
[1]. Bardazzi F, Odorici G,
Virdi A, Antonucci VA, Tengattini V, Patrizi A, et al. Autoantibodies in psoriatic
patients treated with anti-TNF-a therapy. J Dtsch Dermatol Ges 2014;12:401-6.
[2]. Bischoff SC, Mailer R, Pabst O, Weier
G, Sedlik W, Li Z, et al. Role of serotonin in intestinal inflammation: Knockout
of serotonin reuptake transporter exacerbates 2,4,6-trinitrobenzene sulfonic acid
colitis in mice. Am J PhysiolGastrointest Liver Physiol 2009; 296:G685-95.
[3]. Costedio MM, Coates MD, Danielson AB,
Buttolph TR 3rd, Blaszyk HJ, Mawe GM, et al. Serotonin signaling in diverticular
disease. J GastrointestSurg 2008; 12: 1439-45.
[4]. Danese S. New therapies for inflammatory
bowel disease: From the bench to the bedside. Gut 2012; 61:918-32.
[5]. Ghia JE, Li N, Wang H, Collins M, Deng
Y, El-Sharkawy RT, et al. Serotonin has a key role in pathogenesis of experimental
colitis. Gastroenterology 2009; 137:1649-60.
[6]. Haub S, Ritze Y, Bergheim I, Pabst O,
Gershon MD, Bischoff SC. Enhancement of intestinal inflammation in mice lacking
interleukin 10 by deletion of the serotonin reuptake transporter. NeurogastroenterolMotil
2010;22:826-34.
[7]. Levin AD, van den Brink GR. Selective
inhibition of mucosal serotonin as treatment for IBD? Gut 2014; 63:866-7.
[8]. Margolis KG, Pothoulakis C. Serotonin
has a critical role in the pathogenesis of experimental colitis. Gastroenterology
2009; 137:1562-6.
[9]. Margolis KG, Stevanovic K, Li Z, Yang
QM, Oravecz T, Zambrowicz B, et al. Pharmacological reduction of mucosal but not
neuronal serotonin opposes inflammation in mouse intestine. Gut 2014; 63:928-37.
[10]. Morris GP, Beck PL, Herridge MS, Depew
WT, Szewczuk MR, Wallace JL. Hapten-induced model of chronic inflammation and ulceration
in the rat colon. Gastroenterology 1989; 96: 795-803.
[11]. Margolis KG, Stevanovic K, Li Z, Yang
QM, Oravecz T, Zambrowicz B, et al. Pharmacological reduction of mucosal but not
neuronal serotonin opposes inflammation in mouse intestine. Gut 2014;63:928-37.
[12]. Spiller R. Serotonin and GI clinical
disorders. Neuropharmacology 2008; 55:1072-80.
[13]. Xu XR, Liu CQ, Feng BS, Liu ZJ. Dysregulation
of mucosal immune response in pathogenesis of inflammatory bowel disease. World
J Gastroenterol 2014; 20: 3255-64.
[14]. Zhang YZ, Li YY. Inflammatory bowel disease: Pathogenesis. World J Gastroenterol 2014; 20: 91-9.
[15]. Zheng X, Kang A, Dai C, Liang Y, Xie T, Xie L, et al. Quantitative analysis of neurochemical panel in rat brain and plasma by liquid chromatography-tandem mass spectrometry. Anal Chem 2012;84: 10044-51.

