Socio-demographic Factors Influencing the Adoption of Digital Health Tools for Public Health Emergencies in Northern Nigeria
Abstract:
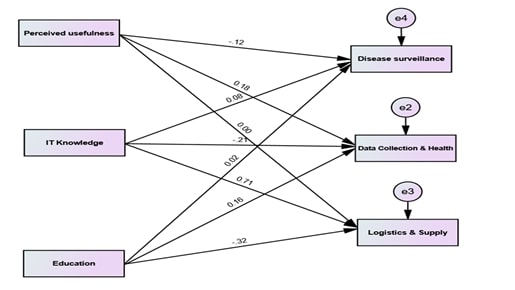
This study assessed the
determinants influencing the adoption of digital health tools for public health
emergencies in primary healthcare centres in Nigeria. The research was
conducted in registered primary healthcare centres located in Abuja-Federal
Capital Territory, Niger, and Nasarawa in Northcentral Nigeria. A multistage
sampling technique was employed, utilizing pretested semi-structured
questionnaire for data collection. The findings revealed the recent
implementation of 11 digital health tools. The tools were classified into
categories: Disease Surveillance and Response Systems, Data Collection,
Analytics, Visualization and Use, and Logistics and Supply Chain Management. Key
factors affecting the adoption of these tools included Age (χ² = 203.64, p <
0.001), Sex (χ² = 136.92, p < 0.001), Marital Status (χ² = 44.64, p <
0.001), Level of Education (χ² = 8.37, p = 0.007), Rate of IT Knowledge (χ² =
228.22, p < 0.001), Profession (χ² = 151.55, p < 0.001), and PHC (χ² =
212.79, p < 0.001). The findings indicate that multiple demographic and
professional factors significantly influence the adoption of digital health
tools. The research identified key factors that affect the effective
implementation and adoption of these technologies. Identified key enablers
comprise robust infrastructure, stakeholder engagement, policy development,
financial sustainability, and user-centred design. By addressing these barriers
and leveraging identified enablers, Nigeria can improve its preparedness and
response to public health emergencies, thereby enhancing healthcare outcomes
and greater equity in health services. This study offered insights and
recommendations for policymakers and practitioners focused on advancing
sustainable digital health initiatives Nigeria.
References:
[1]. UNICEF. 2020. Digital
health and digital engagement for COVID-19 preparedness and response. New York:
UNICEF.
[2]. Federal Government of
Nigeria. 2019. Second National Strategic Health Development Plan 2018-2022.
Federal Government of Nigeria.
[3]. Shuaib, F., Rajni,
G., Musa, E. O., Mahoney, F. J., Oguntimehin, O., Nguku, P. M., Nasidi, A.
2014. Ebola Virus Disease Outbreak — Nigeria, July–September 2014. Atlanta:
Centers for Disease Control and Prevention: Morbidity and Mortality Weekly
Report (MMWR).
[4]. World Health
Organization. 2019. Report of the Global
Conference on Primary Health Care: from Alma-Ata towards universal health
coverage and the (WHO/UHC/SDS/2019.62). Geneva: World Health Organization.
[5]. ITU. 2021. ICTs and
Digital Health. From ITU Web site: https://www.itu.int/en/mediacentre/backgrounders/Pages/icts-digital-health.aspx.
[6]. World Health
Organization. 2016. Monitoring and evaluating digital health interventions: a
practical guide to conducting research and assessment. WHO: Geneva.
[7]. HealthIT. (n.d.).
Public health focuses on preventing disease, diagnosing health conditions, and
promoting health. From HealthIT.gov Web site: https://www.healthit.gov/topic/health-it-health-care-settings/public-health.
[8]. World Health
Organization. 2016. International Health Regulations (2005). (3rd ed.). Geneva:
WHO
[9]. Zayyad, M., &
Toycan, M. (2018). Factors affecting sustainable adoption of e-health
technology in developing countries: an exploratory survey of Nigerian hospitals
from the perspective of healthcare professionals. PeerJ.
[10]. Nieukwerk, v. A.
(2019, August Accessed April 16 2023). Africa’s approaches to crisis management
are unique when it comes to dealing with disease. From World Economic Forum: https://www.weforum.org/agenda/2019/08/how-to-manage-in-a-crisis-lessons-from-the-west-africa-ebola-outbreak/.
[11]. Nigeria Centre for
Disease Control. (2024). An update of cholera outbreak in Nigeria. From NCDC: https://ncdc.gov.ng/diseases/sitreps/?cat=7&name=An%20update%20of%20Cholera%20outbreak%20in%20Nigeria.
[12]. Goode, E., Thomas,
E., & Landeg, O. E. 2021. Development of a Rapid Risk and Impact Assessment
Tool to Enhance Response to Environmental Emergencies in the Early Stages of a
Disaster: A Tool Developed by the European Multiple Environmental Threats
Emergency NETwork (EMETNET) Project. Int J Disaster Risk Sci, 528-539.
[13]. Noah, N. 2021.
Surveillance of Infectious Diseases. Encyclopedia of Virology, 247-55.
[14]. World Health
Organization. 2018. Progress Report on Utilizing E-Health Solutions to Improve
National Health Systems in the African Region. WHO.
[15]. Jameela A, N. M.
2020. Health 4.0: On the Way to Realizing the Healthcare of the Future. IEEE
Access.
[16]. Emnify. 2021. An
Introduction to Industry 4.0. From Emnify Web site: https://www.emnify.com/blog/industry-4-0.
[17]. Khalil, H., & Kynoch, K. 2021. Implementation of
sustainable complex interventions in health care services: the triple C model. BMC
Health Serv Res.
[18]. Probasco, J. 2023. Why Do Healthcare Costs Keep
Rising? From Investopedia Web site: https://www.investopedia.com/insurance/why-do-healthcare-costs-keep-rising/.
[19]. Digital Health
Africa. 2021. Expanding The Scope Of Health Care Services With Effective
Digital Health Technologies. From Digital Health Africa Web site: https://www.biihealthtech.com/digihealthafrica/.
[20]. Olu, O., Muneene, D., Bataringaya, J. E.,Turgeon, Y.
2019. How can digital health technologies contribute to sustainable attainment
of universal health coverage in Africa? A perspective. Front Public Health.
[21]. Karamagi, H., Muneene, D., Droti, B., Jepchumba, V.,
Okeibunor, J., Nabyonga, J., Kipruto, H. 2022. eHealth or e-Chaos: The use
of Digital Health Interventions for Health Systems Strengthening in sub-Saharan
Africa over the last 10 years: A scoping review. J Glob Health.
[22]. Love B. Ayamolowo, L. B., Irinoye, O. O., & Olaniyan,
A. S. 2023. Utilization of electronic health records and associated factors
among nurses in a faith-based teaching hospital,Ilisan, Nigeria. JAMIA Open.
[23]. Akwaowo, C., Sabi, H., Ekpenyong, N., Isiguzo, C., Andem,
N., Maduka, O., . . . Uzoka, F. 2022. Adoption of electronic medical records in
developing countries—A multi-state study of the Nigerian healthcare system. Front.
Digit. Health.
[24]. Ahmed MA, M. M. 2022. Assessment of information
communication technology and eHealth use amongst healthcare providers in
selected primary health centers in Kano, Nigeria. Journal of Basic and
Social Pharmacy Research.
[25]. Sanqui, R., & Declaro-Ruedas, M. 2020. Knowledge and
attitudes towards healthcare information technology of the rural health workers
in SAMARICA, Occidental Mindoro, Philippines. . Asian Journal of Education
and Social Studies.
[26]. Jain, R., Dupare, R., Bhanushali, N., & Kumar, V.
2020. Knowledge and utilization of computer among health-care professionals in
Mumbai. Journal of Indian Association of Public Health Dentistry.
[27]. Shiferaw, K., Tilahun, B., & Endehabtu, B. 2020.
Healthcare providers’ digital competency: a cross-sectional survey in a
low-income country setting. BMC Health Sevices Research.
[28]. World Health Organization. 2023. Sex distribution of
health workers. From WHO Web site: https://apps.who.int/gho/data/node.main.HWFGRP_BYSEX?lang=en.
[29]. World Health Organization. 2018. The invisible boys
and girls: Understanding barriers to accessing healthcare among disadvantaged
Nigerian youth. From WHO Web site: https://www.afro.who.int/news/invisible-boys-and-girls-understanding-barriers-accessing-healthcare-among-disadvantaged.
[30]. Okereke, E. U. 2020. Female clients’ gender preferences
for frontline health workers who provide maternal, newborn and child health
(MNCH) services at primary health care level in Nigeria. BMC Health Serv Res.
[31]. Blondino, C. K. 2024. The use and potential impact of
digital health tools at the community level: results from a multi-country
survey of community health workers. BMC Public Health.
[32]. Sampson, S. U.-J. 2024. Assessment of the compliance with
minimum quality standards by public primary healthcare facilities in Nigeria. Health
Res Policy Sys.
[33]. Ogah, P. U. 2024. Primary health care in Nigeria: best
practices and quality of care in Nigeria. BMC Health Serv Res.
[34]. Ekenna, A., Itanyi, I., Nwokoro, U., Hirschhorn, L. R.,
& Uzochukwu, B. 2020. How ready is the system to deliver primary
healthcare? Results of a primary health facility assessment in Enugu State,
Nigeria. Health Policy and Planning, Pages i97–i106.
[35]. Ojo, et al. 2022. ‘Perception of Healthcare Workers on
the Integration of Electronic Health Records in Primary Health Centers in
Nigeria. CIN - Computers Informatics Nursing, 786-794.
[36]. World Health
Organization. 2024. Digital tools can help improve women’s health and promote
gender equality, WHO report shows. From WHO Web site: https://www.who.int/europe/news/item/08-03-2024-digital-tools-can-help-improve-women-s-health-and-promote-gender-equality--who-report-shows.
[37]. Ibeneme, S., Karamagi, H., Muneene, D., Goswami, K.,
Chisaka, N., & Okeibunor, J. 2022. Strengthening health systems using
innovative digital health technologies in Africa. Frontiers in Digital
Health.
[38]. Kipruto, H., Muneene, D., Droti, B., Jepchumba, V.,
Okeibunor, C. J.-O., & Karamagi, H. C. 2022. Use of Digital Health
Interventions in Sub-Saharan Africa for Health Systems Strengthening Over the
Last 10 Years: A Scoping Review Protocol. Frontiers in Digital Health.
[39]. Owoyemi, A., Osuchukwu, J. I., Azubuike, C., Ikpe, R. K.,
Nwachukwu, B. C., 2022. Digital Solutions for Community and Primary Health
Workers: Lessons From Implementations in Africa. Frontiers in Digital Health.
[40]. Owhor, G. A., Abdulwahab, A. A., Shomuyiwa, D. O., &
Okoli, E. A. 2023. Overview of Digital Health in Sub-Saharan Africa: Challenges
and Recommendations. IOSR Journal of Nursing and Health Science (IOSR-JNHS),
19-21.
[41]. Ravi, N., Thomas, C., & Odogwu, J. 2024. How to reload and upgrade digital health to serve the healthcare needs of Nigerians. Frontiers in Digital Health.

