Ayurveda After Age of Covid-19 Exploring the Impact and Empowering Informed Decisions Through Health Literacy
Abstract:
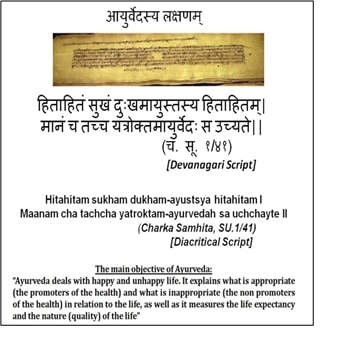
This paper explores the role of
Ayurveda in the post- COVID era, focusing on its potential impact on healthcare
systems and the empowerment of informed decision-making through health
literacy. Ayurveda, an ancient holistic healing system originating in India
over 5,000 years ago, offers a unique approach to health promotion and disease
management based on personalized treatments, herbal medicines, lifestyle modifications,
and preventive care. The COVID-19 pandemic has underscored the importance of
exploring complementary treatments, such as Ayurveda, which provides
immune-boosting techniques, post-COVID symptom management, mental health
support, and integrative healthcare options. By integrating Ayurveda into
mainstream healthcare systems, policymakers and healthcare authorities can
address contemporary health challenges more effectively while promoting greater
health literacy among individuals. This paper discusses the historical
background, principles, and therapeutic modalities of Ayurveda, along with its
potential role in boosting immunity and managing post- COVID symptoms. It also
examines the challenges and opportunities of integrating Ayurveda into
post-pandemic healthcare, including policy recommendations, education reforms,
and industrial initiatives. Overall, the integration of Ayurveda into modern
healthcare systems holds promise for improving healthcare delivery, enhancing
patient outcomes, and fostering greater health literacy in the post- COVID era.
References:
[1]. Jaiswal. S., &
Williams, L. L., (2017). A Glimpse of Ayurveda – the Forgotten History and
Principles of Indian Traditional Medicine. Journal of Traditional and Complementary
Medicine, 7(1), 50–53. https://doi.org/10.1016/j.jtcme.2016.02.002
[2]. Menendez, C., Gonzalez, R., Donnay, F., & Leke, R. G. F.,
(2020). Avoiding Indirect Effects of Covid-19 on Maternal and Child Health. The
Lancet Global Health, 8(7), e863–e864. https://doi.org/10.1016/s2214-109x(20)30239-4
[3]. Abraham Haileamlak. (2021). Editorial Message. Ethiopian
Journal of Health Sciences, 31(1). https://doi.org/10.4314/ejhs.v31i1.1
[4]. Menendez, C., Gonzalez, R., Donnay, F., & Leke, R. G. F.,
(2020). Avoiding Indirect Effects of COVID-19 on Maternal and Child Health. The
Lancet Global Health, 8(7), e863–e864. https://doi.org/10.1016/s2214-109x(20)30239-4
[5]. Park, C., Sugand, K., Nathwani, D., Bhattacharya, R., &
Sarraf, K. M., (2020). Impact of the COVID-19 Pandemic on Orthopedic Trauma Workload
in a London Level 1 Trauma Center: The “Golden Month.” Acta Orthopaedica,
91(5), 556–561. https://doi.org/10.1080/17453674.2020.1783621
[6]. Prajapati, S. K.,
Malaiya, A., Mishra, G., Jain, D., Kesharwani, P., Mody, N., Ahmadi, A.,
Paliwal, R., & Jain, A., (2022). An Exhaustive Comprehension of the Role of
Herbal Medicines in Pre- and Post-Covid Manifestations. Journal of
Ethnopharmacology, 296, 115420. https://doi.org/10.1016/j.jep.2022.115420
[7]. Malagekumbura, M. K., & Biyiri, E. W., (2022). The
Challenges and Potential to Promote Ayurvedic Tourism In Sri Lanka During The
Post-Covid-19 Pandemic.
[8]. Mukherjee, P. K., Harwansh, R. K., Bahadur, S., Banerjee, S.,
Kar, A., Chanda, J., Biswas, S., Ahmmed, Sk. M., & Katiyar, C. K., (2017).
Development of Ayurveda – Tradition to Trend. Journal of Ethnopharmacology,
197, 10–24. https://doi.org/10.1016/j.jep.2016.09.024
[9]. Kizhakkeveettil, A., Parla, J., Patwardhan, K., Sharma, A.,
& Sharma, S. (2023). History, Present and Prospect of Ayurveda. In History,
Present and Prospect of World Traditional Medicine (pp. 1–72). World
Scientific. https://dx.doi.org/10.1142/9789811282171_0001
[10]. Varier, M. R. R., (2020). A Brief History of Ayurveda. Oxford
University Press.
[11]. Kapur, M., (2015). Basic Principles of Ayurveda. In
Psychological Perspectives on Childcare in Indian Indigenous Health Systems
(pp. 15–29). Springer India. https://dx.doi.org/10.1007/978-81-322-2428-0_2
[12]. Ramaswamy, S.,
(2018). Reflections on Current Ayurveda Research. Journal of Ayurveda and
Integrative Medicine, 9(4), 250–251. https://doi.org/10.1016/j.jaim.2018.11.001
[13]. Garba, S., & Mungadi, H. U., (2019). Quantitative
Chemical Compositions of Neem (Azadirachta Indica) Leaf Aqueous Extracts in
Sokoto, Nigeria. International Journal of Research and Scientific Innovation,
6(7), 2-321
[14]. Kuete, V., (Ed.). (2017). Medicinal Spices and Vegetables
from Africa: Therapeutic Potential Against Metabolic, Inflammatory, Infectious
and Systemic Diseases. Academic Press.
[15]. Shrivastava, R., (2020). Immunity Boosters: Solutions from Nature
– Herbs and Spices. Journal of Renal Nutrition and Metabolism, 6(2),
35. https://doi.org/10.4103/jrnm.jrnm_20_20
[16]. Utomo, R. Y., Ikawati, M., & Meiyanto, E., (2020). Revealing
the Potency of Citrus and Galangal Constituents to Halt Sars-Cov-2 Infection.
MDPI AG. https://dx.doi.org/10.20944/preprints202003.0214.v1
[17]. Bashir, F., & Afrin, Z., (2019). Zanjabeel (Zingiber Offcinale)
Transformation of Culinary Spice to a Multi-Functional Medicine. Journal of
Drug Delivery and Therapeutics, 9(4-s), 721–725. https://doi.org/10.22270/jddt.v9i4-s.3299
[18]. Dorra, N., El-Berrawy, M., Sallam, S., & Mahmoud, R.,
(2019). Evaluation of Antiviral and Antioxidant Activity of Selected Herbal Extracts.
Journal of High Institute of Public Health, 49(1), 36–40. https://doi.org/10.21608/jhiph.2019.29464
[19]. Ahkam, A. H., Hermanto, F. E., Alamsyah, A., Aliyyah, I. H.,
& Fatchiyah, F., (2020). Virtual Prediction of Antiviral Potential of Ginger
(Zingiber officinale) Bioactive Compounds Against Spike and MPro of SARS-CoV2
protein. Berkala Penelitian Hayati, 25(2), 52–57. https://doi.org/10.23869/bphjbr.25.2.20207
[20]. Walls, A. C., Park, Y.-J., Tortorici, M. A., Wall, A.,
McGuire, A. T., & Veesler, D., (2020). Structure, Function, and Antigenicity
of the Sars-Cov-2 Spike Glycoprotein. Cell, 181(2), 281-292.e6. https://doi.org/10.1016/j.cell.2020.02.058
[21]. Hajimonfarednejad, M., Ostovar, M., Raee, M. J., Hashempur,
M. H., Mayer, J. G., & Heydari, M., (2019). Cinnamon: A Systematic Review of Adverse Events. Clinical
Nutrition, 38(2), 594–602. https://doi.org/10.1016/j.clnu.2018.03.013
[22]. Lavaee, F., Moshaverinia, M., Rastegarfar, M., &
Moattari, A., (2020). Evaluation of the Effect of Hydro Alcoholic Extract of Cinnamon
on Herpes Simplex Virus-1. Dental Research Journal, 17(2), 114. https://doi.org/10.4103/1735-3327.280889
[23]. Vijayasteltar, L., Nair, G. G., Maliakel, B., Kuttan, R.,
& I.M., K. (2016). Safety Assessment of a Standardized Polyphenolic Extract
of Clove Buds: Subchronic Toxicity and Mutagenicity Studies. Toxicology
Reports, 3, 439–449. https://doi.org/10.1016/j.toxrep.2016.04.001
[24]. Rajagopal, K., Byran, G., Jupudi, S., & Vadivelan, R.,
(2020). Activity of Phytochemical Constituents of Black Pepper, Ginger, and Garlic
Against Coronavirus (COVID-19): An in Silico Approach. International Journal
of Health & Allied Sciences, 9(5), 43. https://doi.org/10.4103/ijhas.ijhas_55_20
[25]. Jamshidi, N., & Cohen, M. M., (2017). The Clinical
Efficacy and Safety of Tulsi in Humans: A Systematic Review of the Literature.
Evidence-Based Complementary and Alternative Medicine, 2017, 1–13. https://doi.org/10.1155/2017/9217567
[26]. Shree, P., Mishra, P., Selvaraj, C., Singh, S. K., Chaube,
R., Garg, N., & Tripathi, Y. B., (2020). Targeting COVID-19 (SARS-CoV-2) Main
Protease Through Active Phytochemicals of Ayurvedic Medicinal Plants – Withania
Somnifera (Ashwagandha), Tinospora Cordifolia (Giloy) and Ocimum Sanctum
(Tulsi) – A Molecular Docking Study. Journal of Biomolecular Structure and
Dynamics, 40(1), 190–203. https://doi.org/10.1080/07391102.2020.1810778
[27]. Mohajer Shojai, T., Ghalyanchi Langeroudi, A., Karimi, V.,
Barin, A., Sadri, N., The Effect of Allium Sativum (Garlic) Extract on Infectious
Bronchitis Virus in Specific Pathogen Free Embryonic Egg. Avicenna J Phytomed.
2016 Jul-Aug;6(4):458-267. PMID: 27516987; PMCID: PMC4967842.
[28]. Alzohairy, M. A., (2016). Therapeutics Role of Azadirachta Indica
(Neem) and Their Active Constituents in Diseases Prevention and Treatment.
Evidence-Based Complementary and Alternative Medicine, 2016, 1–11. https://doi.org/10.1155/2016/7382506
[29]. Ahmad, A., Javed, M. R., Rao, A. Q., & Husnain, T.,
(2016). Designing and Screening of Universal Drug from Neem (Azadirachta
indica) and standard drug chemicals against influenza virus nucleoprotein. BMC
Complementary and Alternative Medicine, 16(1). https://doi.org/10.1186/s12906-016-1469-2
[30]. Ch, R., Muralikumar, V., & Seshachalam, C. (2020). Inhibitory
Effect of Phytochemicals from Azadirachta indica A Juss. and Tinospora
cordifolia (Thunb.) Miers against SARS-CoV-2 M pro and Spike Protease- An In
Silico Analysis. ScienceOpen. http://dx.doi.org/10.14293/s2199-1006.1.sor-.ppi1tym.v1
[31]. S. M. Gopinatha, R. P. (2018). Antiviral prospective of
Tinospora cordifolia on HSV-1. International Journal of Current Microbiology
and Applied Sciences, 7(1), 3617–3624. https://doi.org/10.20546/ijcmas.2018.701.425
[32]. Chowdhury, P., (2020). In Silico Investigation of
Phytoconstituents from Indian Medicinal Herb ‘Tinospora Cordifolia (Giloy)’
Against Sars-Cov-2 (Covid-19) by Molecular Dynamics Approach. Journal of
Biomolecular Structure and Dynamics, 39(17), 6792–6809. https://doi.org/10.1080/07391102.2020.1803968
[33]. Sagar, V., & Kumar, A. H., (2020). Efficacy of Natural
Compounds from Tinospora cordifolia Against SARS-CoV-2 Protease, Surface
Glycoprotein and RNA Polymerase. Biology, Engineering, Medicine and Science
Reports, 6(1), 6–8. https://doi.org/10.5530/bems.6.1.2
[34]. Dasgupta, A., Kalhan, A., & Kalra, S., (2020). Long Term
Complications and Rehabilitation of Covid-19 Patients. Journal of the
Pakistan Medical Association, 0, 1. https://doi.org/10.5455/jpma.32
[35]. Alam, S., Sarker, Md. M. R., Afrin, S., Richi, F. T., Zhao,
C., Zhou, J.-R., & Mohamed, I. N., (2021). Traditional Herbal Medicines,
Bioactive Metabolites, and Plant Products Against Covid-19: Update on Clinical
Trials and Mechanism of Actions. Frontiers in Pharmacology, 12. https://doi.org/10.3389/fphar.2021.671498
[36]. Puthiyedath, R., Gundeti, M., Edamala Narayanan, P. N., &
Narayanam, S., (2023). Learnings from a Veteran Oncologist’s Long-Standing Efforts
in Integrative Oncology. Journal of Ayurveda and Integrative Medicine, 14(1),
100563. https://doi.org/10.1016/j.jaim.2022.100563
[37]. Rastogi, S., Singh, N., & Pandey, P., (2022).
Telemedicine for Ayurveda Consultation: Devising Collateral Methods During the
COVID-19 Lockdown Impasse. Journal of Ayurveda and Integrative Medicine,
13(1), 100316. https://doi.org/10.1016/j.jaim.2020.05.001
[38]. Raman, R., Achuthan, K., Nair, V. K., & Nedungadi, P., (2022). Virtual Laboratories- A Historical Review and Bibliometric Analysis of the Past Three Decades. Education and Information Technologies, 27(8), 11055–11087. https://doi.org/10.1007/s10639-022-11058
[39]. Rattan, T. K., Joshi, M., Vesty, G., & Sharma, S., (2022). Sustainability Indicators in Public Healthcare: A Factor Analysis Approach. Journal of Cleaner Production, 370, 133253. https://doi.org/10.1016/j.jclepro.2022.133253
[40]. Katoch, D., and Sharma, J. S., Banerjee, S., Biswas, R., Das,
B., Goswami, D., Harwansh, R. K., Katiyar, C. K., & Mukherjee, P. K.,
(2017). Government Policies and Initiatives for Development of Ayurveda. Journal
of Ethnopharmacology, 197, 25–31. https://doi.org/10.1016/j.jep.2016.08.018

