Effects of Enhance Adherence Counselling on Viral Load Suppression Among High Viral Load HIV Seropositive Patients in a Nigerian Tertiary Health Facility
Abstract:
Background: EAC helps clients
overcome adherence hurdles and improve ART adherence. This study examines the
effect of EAC on viral load suppression. Method: This quantitative study aims
to determine the impacts of enhanced adherence counselling (EAC) on viral load
in Defence Headquarters Medical Center, Abuja, Nigeria. The medical records of
HIV clients on ART included in EAC were extracted from the hospital and
analyzed to determine the impacts of EAC on viral loads suppression of clients
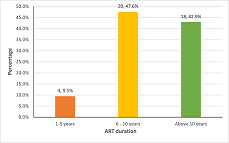
in the program. Result: Almost half of the PLWHIV in EAC have been on ART for
6-10 years (47.6%), 42.9% for more than ten years, and 9.5% have been on ART
for 1 – 5 years. 76.2% of respondents were on the 1st line of the ART regimen,
while 23.8% were on the 2nd line. 97.6% of clients enrolled for EAC were at the
WHO stage I HIV infection, and only one (2.4%) was in stage IV. 50% tested for
viral load was due to viral blip, 28.6% due to unsuppressed viral load and
21.4% were tested to monitor their VL. Furthermore, of the 33 clients with
viral load results, 14 (42.4%) had very low-level viremia (<50 copies/ml),
10 (30.3%) had low-level viremia (50–1000 copies/ml), but 9 (27.3%) still had
high-level viremia (>1000 copies/ml). 42.9% enrolled for EAC because of pill
burdens, 31.0% due to irregular dosing frequency, 19.0% because of pill social
problems, and 2.1% were people lost to follow-up returned..
Keywords: Antiretroviral therapy, EAC, Viral load.
References:
[1] WHO.
Adapting and Implementing New Recommendations on HIV Patient Monitoring.
Geneva, Switzerland, 2017. 2017.
[2] Ministry
of Health Uganda. Uganda Clinical Guidelines 2016. Retrieved on 21/6/2018.
Minist Heal Uganda [Internet]. 2016;1–1142. Available from: http://health.go.ug/content/uganda-clinical-guidelines-2016.
[3] WHO.
Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and
Preventing HIV Infection. Recommendations for a Public Health Approach.
2016;(2nd ed):1–429.
[4] MoH.
National Training Curriculum for Roll Out of the Consolidated Guidelines for
the Prevention and Treatment of Hiv and Aids in Uganda, 2020. 2020;142–170.
[5] Diress
G, Dagne S, Alemnew B, Adane S, Addisu A. Viral Load Suppression after Enhanced
Adherence Counseling and Its Predictors among High Viral Load HIV Seropositive
People in North Wollo Zone Public Hospitals, Northeast Ethiopia, 2019:
Retrospective Cohort Study. AIDS Res Treat. 2020;2020.
[6] Nasuuna
E, Kigozi J, Babirye L, Muganzi A, Sewankambo NK, Nakanjako D. Low HIV viral
suppression rates following the intensive adherence counseling (IAC) program
for children and adolescents with viral failure in public health facilities in
Uganda. BMC Public Health. 2018;18(1).
[7] Usman
S, Oluwaniyi O, Olubayo G, Akinmurele T, Agboola G, Abodunde F, et al. 90-90-90
Ambitious Targets: Achieving the Last 90 of the UNAIDS Targets in Western
Nigeria. Int STD Res Rev. 2017;6(2):1–9.
[8] Fatunsi
E, Ariyo A, Suraju A, Oguejiofor I, Tomori M, Owolagba FE, et al. The progress
towards achieving the UNAIDS ambitious viral suppression target among adults
living with HIV in South-Western Nigeria. 2020;2(1):8–12.
[9] Villa
africa reality. Abuja - FCT | All About Nigeria’s Federal Capital City.
2021;1–1. Available from: https://www.villaafrika.com/fct-abuja-city-profile/.
[10] World
Population. Review Abuja population 2021. 2021.
[11] Naiis.
Nigeria Prevalence Rate - NACA Nigeria [Internet]. 2019 [cited 2021 Oct 18]. p.
1–1. Available from: https://naca.gov.ng/nigeria-prevalence-rate/.
[12] Hernán
MA. The effect of combined antiretroviral therapy on the overall mortality of
HIV-infected individuals. Aids. 2010;24(1):123–37.
[13] Bock
NN, Emerson RC, Reed JB, Nkambule R, Donnell DJ, Bicego GT, et al. Changing
antiretroviral eligibility criteria: Impact on the number and proportion of
adults requiring treatment in Swaziland. J Acquir Immune Defic Syndr
[Internet]. 2016;71(3):338–44. Available from: https://doi.org/10.1097/QAI.0000000000000846%0APMID:26361174.
[14] Loutfy
MR, Wu W, Letchumanan M, Bondy L, Antoniou T, Margolese S, et al. Systematic
Review of HIV Transmission between Heterosexual Serodiscordant Couples where
the HIV-Positive Partner Is Fully Suppressed on Antiretroviral Therapy. PLoS
One [Internet]. 2013;8(2). Available from: https://doi.org/10.1371/journal.pone.%0A0055747
PMID: 23418455. Erratum in.
[15] Attia
S, Egger M, Müller M, Zwahlen M, Low N. Sexual transmission of HIV according to
viral load and antiretroviral therapy: Systematic review and meta-analysis.
Aids. 2009;23(11):1397–404.
[16] Jain
V, Byonanebye DM, Amanyire G, Kwarisiima D, Black D, Kabami J, et al.
Successful antiretroviral therapy delivery and retention in care among
asymptomatic individuals with high CD4+T-cell counts above 350 cells/ml in
rural Uganda. Aids [Internet]. 2014;28(15):2241–9. Available from: https://doi.org/10.1097/QAD.%0A0000000000000401
PMID: 25022596.
[17] Hall
HI, Tang T, Westfall AO, Mugavero MJ. HIV care visits and time to viral
suppression, 19 U.S. jurisdictions, and implications for treatment, prevention
and the National HIV/AIDS Strategy. Plos One. 2013;8(12).
[18] World
Health Organization. Guideline on When To Start Antiretroviral Therapy and on
Pre-Exposure Prophylaxis for HIV. Geneva World Heal Organ.
2015;(September):1–76.
[19] Priscilla
F., Mlay A. Factors associated with viral load suppression among HIV/AIDS adult
patients on art medication. A case of Kisarawe district, pwani region. 2019.
[20] Wakooko
P, Gavamukulya Y, Wandabwa JN. Viral load Suppression and Associated Factors
among HIV Patients on Antiretroviral Treatment in Bulambuli District, Eastern
Uganda : A Retrospective Cohort Study. 2020.
[21] Rangarajan
S, Colby DJ, Giang LT, Bui DD, Hung Nguyen H, Tou PB, et al. Factors associated
with HIV viral load suppression on antiretroviral therapy in Vietnam. J Virus Erad.
2016;2(2):94–101.
[22] Awolude
OA, Olaniyi O, Moradeyo M, Abiolu J. Virologic Outcomes Following Enhanced
Adherence Counselling among Treatment Experienced HIV Positive Patients at
University College Hospital, Ibadan, Nigeria. 2021;10(1):53–65.
[23] Diress
G, Dagne S, Alemnew B, Adane S, Addisu A. Viral Load Suppression after Enhanced
Adherence Counseling and Its Predictors among High Viral Load
HIV Seropositive People in North Wollo Zone Public Hospitals, Northeast
Ethiopia, 2019 : Retrospective Cohort Study. 2020;2020.
[24] Geretti
AM, Smith C, Haberl A, Garcia-Diaz A, Nebbia G, Johnson M, et al. Determinants
of virological failure after successful viral load suppression in first-line
highly active antiretroviral therapy. Antivir Ther. 2008;13(7):927–36.
[25] Peltzer
K, Friend-Du Preez N, Ramlagan S, Anderson J. Antiretroviral treatment
adherence among HIV patients in KwaZulu-Natal, South Africa. BMC Public Health.
2010;10.
[26] NIAID.
10 Things to Know About HIV Suppression | NIH: National Institute of Allergy
and Infectious Diseases [Internet]. 2020 [cited 2023 Jan 26]. p. 1–5. Available
from: https://www.niaid.nih.gov/diseases-conditions/10-things-know-about-hiv-suppression.
[27] Brooks
K, Diero L, DeLong A, Balamane M, Reitsma M, Kemboi E, et al. Treatment failure
and drug resistance in HIV-positive patients on tenofovir-based first-line
antiretroviral therapy in western Kenya. J Int AIDS Soc.
2016;19(1).
[28] Anne
L, Jobanputra K, Parker LA, Azih C, Okello V, Maphalala G. Factors Associated
with Virological Failure and Suppression after Enhanced Adherence Counselling,
in Children, Adolescents and Adults on Antiretroviral Therapy for HIV in
Swaziland Authors Factors Associated with Virological Failure and Suppression
afte. 2021;
[29] Talent Bvochora Id, Id SS, Takarinda KC, Bara H. Enhanced adherence counselling and viral load suppression in HIV seropositive patients with an initial high viral load in Harare, Zimbabwe : Operational issues. 2019;444:1–13.

